Lung cancer
Lung cancer
What is Lung Cancer
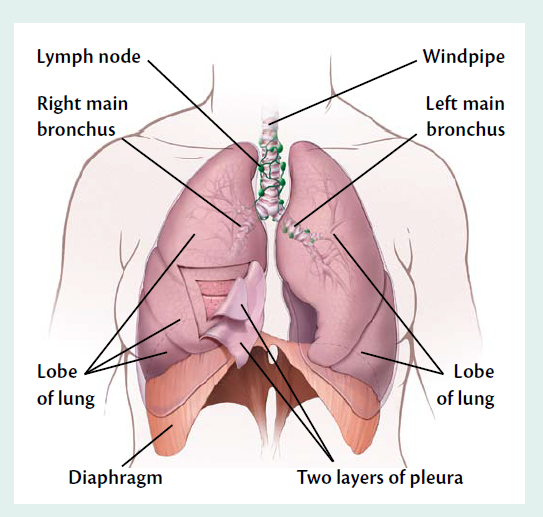
Cancer begins in cells, the building blocks that make up all tissues and organs of the body, including the lungs.
Normal cells in the lungs and other parts of the body grow and divide to form new cells as they are needed. When normal cells grow old or get damaged, they die, and new cells take their place.
Sometimes, this process goes wrong. New cells form when the body doesn’t need them, and old or damaged cells don’t die as they should. The buildup of extra cells often forms a mass of tissue called a growth or tumor.
Tumors in the lung can be benign (not cancer) or malignant (cancer):
Benign tumors
- Are rarely a threat to life
- Don’t invade the tissues around them
- Don’t spread to other parts of the body
- Usually don’t need to be removed
Malignant tumors (lung cancer)
- May be a threat to life
- Can invade nearby organs and tissues
- Can spread to other parts of the body
- Often can be removed but may grow back
Lung cancer cells can spread by breaking away from a lung tumor. They can travel through blood vessels or lymph vessels to reach other parts of the body. After spreading, cancer cells may attach to other tissues and grow to form new tumors that may damage those tissues.
When lung cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the primary (original) tumor. For example, if lung cancer spreads to the bones, the cancer cells in the bones are actually lung cancer cells. The disease is metastatic lung cancer, not bone cancer. For that reason, it is treated as lung cancer, not bone cancer.
Types of Lung Cancer
Lung cancers, also known as bronchogenic carcinomas ("carcinoma" is another term for cancer), are broadly classified into two types: small cell lung cancers (SCLC) ,Non-small cell lung cancers (NSCLC). This classification is based upon the microscopic appearance of the tumor cells. These two types of cancers grow, spread, and are treated in different ways, so a distinction between these two types is important.
Small cell lung cancer
The cells of small cell lung cancer look small under a microscope. SCLC comprises about 10%-15% of lung cancers. This type of lung cancer is the most aggressive and rapidly growing of all the types. SCLC is strongly related to cigarette smoking. SCLCs metastasize rapidly to many sites within the body and are most often discovered after they have spread extensively.
Non-small cell lung cancer
The cells of non-small cell lung cancer are larger than the cells of small cell lung cancer. It doesn’t grow and spread as fast as small cell lung cancer, and it’s treated differently. is the most common lung cancer, accounting for about 85% of all cases. NSCLC has three main types designated by the type of cells found in the tumor.
Adenocarcinomas
Adenocarcinomas re the most common type of NSCLC in the U.S. and comprise up to 40% of lung cancer cases. While adenocarcinomas are associated with smoking like other lung cancers, this type is also seen in non-smokers -- especially women -- who develop lung cancer. Most adenocarcinomas arise in the outer, or peripheral, areas of the lungs. They also have a tendency to spread to the lymph nodes and beyond. Adenocarcinoma in situ (previously called bronchioloalveolar carcinoma) is a subtype of adenocarcinoma that frequently develops at multiple sites in the lungs and spreads along the preexisting alveolar walls. It may also look like pneumonia on a chest X-ray. It is increasing in frequency and is more common in women. People with this type of lung cancer tend to have a better prognosis than those with other types of lung cancer.
Squamous cell carcinomas
Squamous cell carcinomas wre formerly more common than adenocarcinomas; today, they account for about 25% to 30% of all lung cancer cases. Also known as epidermoid carcinomas, squamous cell cancers arise most frequently in the central chest area in the bronchi. This type of lung cancer most often stays within the lung, spreads to lymph nodes, and grows quite large, forming a cavity.
Large cell carcinomas
Large cell carcinomas sometimes referred to as undifferentiated carcinomas, are the least common type of NSCLC, accounting for 10%-15% of all lung cancers. This type of cancer has a high tendency to spread to the lymph nodes and distant sites.
Other types of cancers
can arise in the lung; these types are much less common than NSCLC and SCLC and together comprise only 5%-10% of lung cancers:
Bronchial carcinoids
Bronchial carcinoids account for up to 5% of lung cancers. These tumors are generally small (3-4 cm or less) when diagnosed and occur most commonly in persons under age 40. Unrelated to cigarette smoking, carcinoid tumors can metastasize, and a small proportion of these tumors secrete hormone-like substances. Carcinoids generally grow and spread more slowly than bronchogenic cancers, and many are detected early enough to be surgically removed.
Cancers of supporting lung tissue
Cancers of supporting lung tissue such as smooth muscle, blood vessels, or cells involved in the immune response are rare in the lung.
As discussed previously, metastatic cancers from other primary tumors in the body are often found in the lung. Tumors from anywhere in the body may spread to the lungs either through the bloodstream, through the lymphatic system, or directly from nearby organs. Metastatic tumors are most often multiple, scattered throughout the lung and concentrated in the outer areas rather than central areas of the organ.
Molecular classification
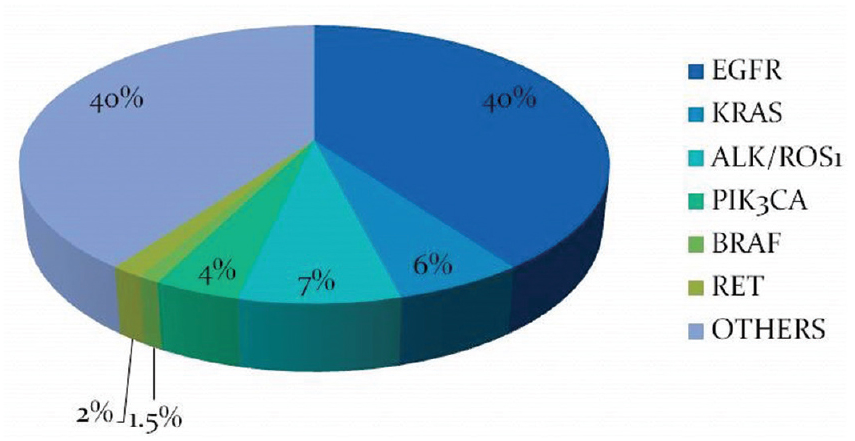
Lung cancer specific mutations (EGFR, KRAS, MET, ERBB2, TP53, STK11, ROS1, RET, NF1, PIK3CA for adenocarcinomas and FGFR1, FGFR2, FGFR3, TP53, STK11, EGFR for squamous cell carcinomas).
Risk factor of lung cancer
A number of factors may increase your risk of lung cancer. Some risk factors can be controlled, for instance, by quitting smoking. And other factors can't be controlled, such as your family history.
Risk factors for lung cancer include:
Smoking.
Your risk of lung cancer increases with the number of cigarettes you smoke each day and the number of years you have smoked. Quitting at any age can significantly lower your risk of developing lung cancer.
Exposure to secondhand smoke.
Even if you don't smoke, your risk of lung cancer increases if you're exposed to secondhand smoke.
Exposure to radon gas.
Radon is produced by the natural breakdown of uranium in soil, rock and water that eventually becomes part of the air you breathe. Unsafe levels of radon can accumulate in any building, including homes.
Radon testing kits, which can be purchased at home improvement stores, can determine whether levels are safe. If unsafe levels are discovered, remedies are available.
Exposure to asbestos and other carcinogens.
Workplace exposure to asbestos and other substances known to cause cancer — such as arsenic, chromium and nickel — also can increase your risk of developing lung cancer, especially if you're a smoker.
Family history of lung cancer.
People with a parent, sibling or child with lung cancer have an increased risk of the disease.
Symptoms of lung cancer
Your doctor may suspect lung cancer if a routine physical exam reveals:
- item Swollen lymph nodes above the collarbone
- item Weak breathing
- item Abnormal sounds in the lungs
- item Dullness when the chest is tapped
- item Unequal pupils
- item Droopy eyelids
- item Weakness in one arm
- item Expanded veins in the arms, chest, or neck
- item Swelling of the face
Some lung cancers produce abnormally high blood levels of certain hormones or substances such as calcium. If a person shows such evidence and no other cause is apparent, a doctor should consider lung cancer.
Lung cancer, which originates in the lungs, can also spread to other parts of the body, such as distant bones, the liver, adrenal glands, or the brain. It may be first discovered in a distant location, but is still called lung cancer if there is evidence it started there.
Diagnosis & Tests
Sputum Cytology
This test looks for cancer cells in your mucus. To get a sample, you'll breathe deeply and then cough with enough force to bring some up from your lungs. Then you'll spit it out into a cup.
Chest X-ray
It uses radiation in low doses to make images of your lungs. It might be the first test you get. If your doctor sees something that looks like cancer, you might need more exams.
CT scan
An x-ray machine linked to a computer takes a series of detailed pictures of your chest, abdomen, brain, or other parts of your body. You’ll receive contrast material by injection into a blood vessel in your arm or hand. For a CT scan of the abdomen, you may receive contrast material by mouth also. The contrast material makes abnormal areas easier to see. The pictures from a CT scan can show the lung tumor’s size. The pictures can also show cancer that has spread to your liver, adrenal glands, brain, or other organs.
PET scan
Your doctor may use a PET scan to get a better view of the tumor in the lung or to find cancer that has spread. You’ll receive an injection of a small amount of radioactive sugar. A machine makes computerized pictures of the sugar being used by cells in the body. Because cancer cells use sugar faster than normal cells, areas with cancer cells look brighter on the pictures.
MRI
A strong magnet linked to a computer is used to make detailed pictures of your head or spine. An MRI can show whether cancer has spread to these areas. Sometimes contrast material is used to make abnormal areas show up more clearly on the picture.
Bone scan
A small amount of a radioactive substance will be injected into a blood vessel. The radioactive substance travels through your bloodstream and collects in the bones. A machine called a scanner detects and measures the radiation. The scanner makes pictures of your bones. Because higher amounts of the radioactive
Needle biopsy or needle aspiration
Your doctor numbs your skin and uses a needle to remove a sample of tissue.
Open biopsy
You need to be in a hospital operating room to get this done.A surgeon removes tissue through a cut in your chest. You'll get anesthesia that puts you to sleep while this is going on.
Blood test
A blood test is a laboratory analysis performed on a blood sample that is usually extracted from a vein in the arm using ahypodermic needle, or via fingerprick.
Stage of Lung cancer
The stage of lung cancer depends mainly on:
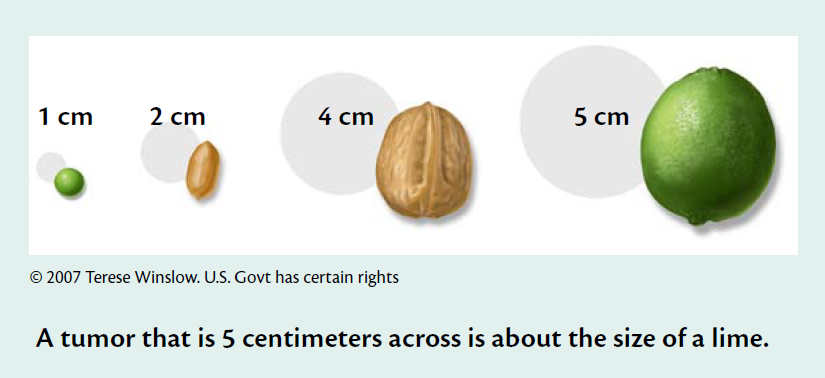
- item The size of the lung tumor
- item How deeply the tumor has invaded nearby tissue, such as the chest wall
- item Whether lung cancer cells have spread to lymph nodes or other parts of the body
Stages of Non-small Cell Lung Cancer
Doctors describe the stages of non-small cell lung cancer using the Roman numerals I, II, III, and IV. Stage I is early-stage cancer, and Stage IV is advanced cancer that has spread to other parts of the body, such as the bones.
Occult Stage Lung Tumor
Tumor cells are found in sputum, but CT scans and other imaging tests don’t show a lung tumor.
Stage 0 Lung Tumor
Abnormal cells are found only in the innermost lining of
the lung. The tumor has not grown through this lining.
A Stage 0 tumor is also called carcinoma in situ. It is not
an invasive cancer.
Stage I Lung Cancer
The lung tumor is an invasive cancer. It has grown through the innermost lining of the lung into deeper lung tissue. The tumor is surrounded by normal tissue, and it doesn’t invade nearby tissues, such as the chest wall.
The tumor is no more than 5 centimeters (about 2 inches) across. Cancer cells are not found in nearby lymph nodes.
Stage II Lung Cancer
The lung tumor is smaller than 7 centimeters across, and cancer cells are found in nearby lymph nodes.
Or, cancer cells are not found in nearby lymph nodes. The lung tumor is more than 5 centimeters across, or it invades nearby tissues, such as the chest wall, diaphragm, pleura, main bronchus, or tissue that surrounds the heart. More than one malignant tumor may be found within the same lobe of the lung.
Stage III Lung Cancer
The tumor may be any size. More than one malignant tumor may be found within the lung.
Cancer cells may be found in lymph nodes on either side of the chest or the neck. The tumor may have invaded nearby organs, such as the heart, esophagus, or trachea.
Stage IV Lung Cancer
Malignant tumors are found in both lungs. Or, the lung cancer has spread to other parts of the body, such as the brain, bones, liver, or adrenal glands. Or, cancer cells are found in fluid between the two layers of pleura. (See page 1 for picture of pleura.)
Stages of Small Cell Lung Cancer
Most doctors describe the stages of small cell lung cancer with two stages:
Limited stage
Cancer is found only on one side of the chest.
Extensive stage
Cancer is found in the lung and also in tissues on the other side of the chest. Or, lung cancer is found in distant organs, such as the brain, or in fluid between the two layers of pleura. (See page 1 for picture of pleura.)
Treatment
The treatment that’s right for you depends mainly on the type and stage of lung cancer. You may receive more than one type of treatment.
At any stage of lung cancer, care is available to control pain and manage breathing problems, to relieve the side effects of treatment, and to ease emotional concerns.
People with lung cancer have many treatment options. Treatment options include:
Surgery
Surgery may be an option for people with early-stage lung cancer.
The surgeon usually removes only the part of the lung that contains cancer. Most people who have surgery for lung cancer will have the lobe of the lung that contains the cancer removed. This is a lobectomy. In some cases, the surgeon will remove the tumor along with less tissue than an entire lobe, or the surgeon will remove the entire lung. The surgeon also removes nearby lymph nodes.
After lung surgery, air and fluid will collect in the chest. A chest tube that was inserted during surgery will allow the fluid to drain. Also, a nurse or respiratory therapist will teach you coughing and breathing exercises. You’ll need to do these exercises several times a day. The chest tube will be removed a few days after surgery.
The time it takes to heal after surgery is different for everyone. Your hospital stay may be a week or longer. It may be several weeks before you return to normal activities.
Radiation therapy
Radiation therapy is an option for people with any stage of lung cancer:
People with early lung cancer may choose radiation therapy instead of surgery.
After surgery, radiation therapy can be used to destroy any cancer cells that may remain in the chest.
In advanced lung cancer, radiation therapy may be used with chemotherapy.
Radiation therapy can be used to help shrink a tumor that is blocking the airway.
Radiation therapy can be used to help relieve pain from lung cancer that has spread to the bones or other tissues.
Radiation therapy is often used to treat lung cancer that has spread to the brain.
The radiation comes from a large machine. The machine aims high-energy rays at your body to kill cancer cells. The treatment affects cells only in the area being treated, such as the chest area.
Although radiation therapy is painless, it may cause other side effects. The side effects depend mainly on how much radiation is given and the part of your body that is treated. Ask your health care team to describe the side effects that you might expect during or after radiation therapy.
Radiation therapy aimed at the chest may cause a sore throat, cough, or shortness of breath. When you try to swallow, you may feel a lump in your throat or burning in your chest or throat. Your health care team can suggest ways to manage these problems. The problems usually go away when treatment ends.
It’s common for the skin in the chest area to become red and dry and to get darker. Sometimes the skin may feel tender or itchy. Check with your doctor before using lotion or cream on your chest. After treatment is over, the skin will heal.
You’re likely to become tired during radiation therapy, especially in the later weeks of treatment. Although getting enough rest is important, most people say they feel better when they exercise every day. Try to go for a short walk, do gentle stretches, or do yoga.
Chemotherapy
Chemotherapy may be used alone, with radiation therapy, or after surgery.
Chemotherapy uses drugs to kill cancer cells. The drugs for lung cancer are usually given directly into a vein (intravenous) through a thin needle.
You’ll probably receive chemotherapy in a clinic or at the doctor’s office. People rarely need to stay in the hospital during treatment.
The side effects depend mainly on which drugs are given and how much. Chemotherapy kills fast-growing cancer cells, but the drugs can also harm normal cells that divide rapidly:
Blood cells: When drugs lower the levels of healthy blood cells, you’re more likely to get infections, bruise or bleed easily, and feel very weak and tired. Your health care team will check for low levels of blood cells. If your levels are low, your health care team may stop the chemotherapy for a while or reduce the dose of the drug. There are also medicines that can help your body make new blood cells.
Cells in hair roots: Chemotherapy may cause hair loss. If you lose your hair, it will grow back after treatment, but the color and texture may be changed.
Cells that line the digestive tract: Chemotherapy can cause a poor appetite, nausea and vomiting, diarrhea, or mouth and lip sores. Your health care team can give you medicines and suggest other ways to help with these problems.
Targeted therapy
People with non-small cell lung cancer that has spread may receive a type of treatment called targeted therapy. Several kinds of targeted therapy are used for non-small cell lung cancer. One kind is used only if a lab test on the cancer tissue shows a certain gene change. Targeted therapies can block the growth and spread of lung cancer cells.
Depending on the kind of drug used, targeted therapies for lung cancer are given intravenously or by mouth. The drug enters the bloodstream and can affect cancer cells all over the body.
During treatment, your health care team will watch you for side effects. You may get a skin rash, diarrhea, or mouth sores, or you may feel very tired. Other possible side effects include shortness of breath, belly pain, high blood pressure, vomiting, and swollen feet and hands. The side effects usually go away after treatment ends.
Immunotherapy
Immunotherapy has the potential to benefit lung cancer patients for whom more conventional chemotherapy or radiation treatments are ineffective. Currently, there are several targeted antibodies approved for lung cancer patients, in addition to three checkpoint immunotherapy drugs. Immune checkpoint therapies include the monoclonal antibody blockade of the cytotoxic T-lymphocyte antigen-4 (CTLA-4) with ipilimumab, as well as antibody blockade of the programmed cell death-1 (PD-1) receptor and the PD-1 ligand. These immune checkpoint therapies have been evaluated in both non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) with early evidence of activity. Vaccines include antigen specific therapies which induce specific antitumor immunity against relevant tumor-associated antigens.
lung cancer related genes
The detection genes suggested in NCCN clinical guidelines for non-small cell lung cancer include EGFR mutation, KRAS mutation, BRAF mutation, ALK fusion, MET mutation and amplification, ROS1 fusion, and ERBB2 mutation.
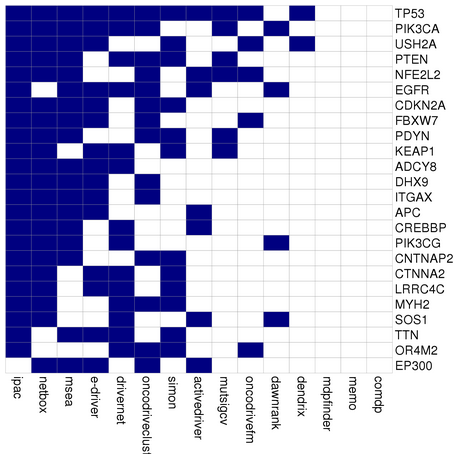
Driver gene (DriverDB by 5 tools)
lung cancer Drugs
Lung Cancer Clinical Trials
Clinical trials are a way to try new medications and treatments that researchers are testing. The goal is to find out how well these treatments work and what side effects they could have.
People with lung cancer who participate in lung cancer clinical trials get the most effective therapy that’s already available, or they may receive new lung cancer treatments that are being tested for future use.
You can ask your doctor to help you find a clinical trial, what’s involved, and what to consider -- for instance, if you’d need to travel to take part. You can also check these websites for information.
Eviti Clinical Trials
This website, developed by the nonprofit Coalition of Cancer Cooperative Groups, is the leading cancer clinical trial search engine. You can search for cancer trials based on disease and location.
National Cancer Institute
This website lists more than 6,000 cancer clinical trials and explains what to do when you find one that you think is right for you.
ClinicalTrials.gov
This website, a service of the National Institutes of Health, is a database of clinical studies worldwide.
CenterWatch
This web site lists industry-sponsored clinical trials that are recruiting patients.
Side Effects
Your health care team can describe your treatment options, the expected results of each option, and the possible side effects. Because cancer treatments often damage healthy cells and tissues, side effects are common. These side effects depend on many factors, including the type of treatment.
As you get ready to start treatment, it’s normal to feel nervous about side effects you might face. To help you prepare, here’s a treatment-by-treatment guide to the most common ones.
Keep in mind that side effects vary even between two people on the same treatment. That's because every person -- and every cancer case -- is unique. The good news is most side effects are temporary and there are ways you can manage them.
Surgery
Pain and weakness. Your doctor will prescribe medication to relieve your pain, but you’ll need to allow time to rest and heal. It’s a good idea to keep a journal so you can track and describe your symptoms. If it gets worse, work with your doctor to adjust medications and fine-tune the dosage.
Chemotherapy
Shortness of breath. You may feel this even though you’re getting enough oxygen and you can breathe normally. It’s how your brain processes chest pain. It should get better overthe next few weeks as you heal. If your lungs are in good shape (other than the cancer) you can usually return to normal life after a while -- even if an entire lung was removed. If you also have a non-cancerous lung disease like emphysema or chronic bronchitis, you may always feel short of breath with some types of activity.
Nausea and vomiting. Feeling like you're going to throw up or actually doing it can be a problem on treatment days. Your doctor will give you medicine to keep these symptoms at bay.
Hair loss. Follicles, the tiny structures that hair grows out of, contain some of the fastest-growing cells in your body. So chemo attacks them, too. Within a few weeks of starting treatment, you may lose some or all of your hair. The good news is that it's almost always temporary. It can make you feel better to cut or shave before it starts to fall out. If you opt to go bald, use an electric shaver so you don't cut your scalp. If you get a wig, shop for it while you still have hair so you can match it to your current hair color.
Bleeding or clotting problems. Platelets are blood cells that help stop bleeding. They plug damaged blood vessels and help your blood clot. If you don't have enough of them, you may bleed or bruise more easily than usual, even from a minor injury. Your doctor will check your platelet count often during your treatment. If it falls too low, you may need a transfusion.
Loss of appetite. Instead of three large meals per day, have five or six small ones. Avoid greasy, salty, sweet, or spicy food that might make you feel queasy. If even the smell of food is a turnoff, eat cold meals instead.
Diarrhea. Frequent bowel movements that are loose or watery can get in the way of your daily life. They can also drain too much liquid from your body. Skip dairy and high-fiber, greasy, or spicy foods. Drink water or suck on ice chips, and call you doctor if your symptoms last more than a day.
Radiation Therapy
- item Shortness of breath
- item Fatigue
- item Nausea and vomiting
- item Diarrhea
- item Hair loss
- item Loss of appetite
- item Skin changes in the area being treated.
- item Sore throat.
Targeted Therapy
Skin problems. You might have rashes. Tell your doctor if you notice any skin changes. If you don’t treat them, they can get worse and lead to infections.
High blood pressure. Your doctor will watch your readings closely if you are getting a drug that can cause this reaction.
Heart damage. Your doctor will test your heart before treatment and watch your condition closely.
Immunotherapy
The newest approach to lung cancer treatment uses drugs to help your immune system spot and destroy cancer cells better. It shows great promise when traditional treatments fail, especially for people whose cancer is in a later stage.
The most common side effects are flu-like symptoms, fatigue, rashes, fever, and drops in blood pressure. But immunotherapy is very new, so doctors still aren’t sure which side effects will happen or how serious they may be.
Nutrition of the patients
Eating well is important before, during, and after cancer treatment. You need the right amount of calories to maintain a good weight. You also need enough protein to keep up your strength. Eating well may help you feel better and have more energy.
Sometimes, especially during or soon after treatment, you may not feel like eating. You may be uncomfortable or tired. You may find that foods don’t taste as good as they used to. In addition, poor appetite, nausea, vomiting, mouth blisters, and other side effects of treatment can make it hard for you to eat.
Your doctor, a registered dietitian, or another health care provider can suggest ways to help you meet your nutrition needs.
Follow-up Care
You’ll need regular checkups (such as every 6 months) after treatment for lung cancer. Checkups help ensure that any changes in your health are noted and treated if needed. If you have any health problems between checkups, contact your doctor.
Lung cancer may come back after treatment. Your doctor will check for the return of cancer. It may return in the chest or it may return in another part of the body, such as the bones.
Checkups also help detect health problems that can result from cancer treatment.
Checkups may include a physical exam, blood tests, or CT scans.