Colorectal cancer
Colorectal cancer
What is Colorectal cancer
Colorectal cancer is a cancer that starts in the colon or the rectum. These cancers can also be named colon cancer or rectal cancer, depending on where they start. Colon cancer and rectal cancer are often grouped together.
Cancer starts when cells in the body begin to grow out of control. Cells in nearly any part of the body can become cancer, and can spread to other areas of the body.

Types of Colorectal cancer
Most colorectal cancers begin as a growth called a polyp on the inner lining of the colon or rectum Some types of polyps can change into cancer over the course of several years, but not all polyps become cancer. The chance of changing into a cancer depends on the kind of polyp. The 2 main types of polyps are:
Adenomatous polyps (adenomas)
These polyps sometimes change into cancer. Because of this, adenomas are called a pre-cancerous condition.
Hyperplastic polyps and inflammatory polyps
These polyps are more common, but in general they are not pre-cancerous.
Other polyp characteristics that can increase the chances a polyp may contain cancer or increase someone’s risk of developing colorectal cancer besides the type include the size (larger than 1cm), the number found (more than two), and if dysplasia is seen in the polyp after it is removed.
Dysplasia, another pre-cancerous condition, is an area in a polyp or in the lining of the colon or rectum where the cells look abnormal (but not like true cancer cells).
If cancer forms in a polyp, it can eventually begin to grow into the wall of the colon or rectum.
The wall of the colon and rectum is made up of several layers. Colorectal cancer starts in the innermost layer (the mucosa) and can grow outward through some or all of the other layers. When cancer cells are in the wall, they can then grow into blood vessels or lymph vessels (tiny channels that carry away waste and fluid). From there, they can travel to nearby lymph nodes or to distant parts of the body.
Molecular classification
Colorectal cancer is a disease originating from the epithelial cells lining the colon or rectum of the gastrointestinal tract, most frequently as a result of mutations in the Wnt signaling pathwaythat increase signaling activity. The mutations can be inherited or acquired, and most probably occur in the intestinal crypt stem cell. The most commonly mutated gene in all colorectal cancer is the APC gene, which produces the APC protein. The APC protein prevents the accumulation of ¦Â-catenin protein. Without APC, ¦Â-catenin accumulates to high levels and translocates (moves) into the nucleus, binds to DNA, and activates the transcription of proto-oncogenes. These genes are normally important for stem cell renewal and differentiation, but when inappropriately expressed at high levels, they can cause cancer. While APC is mutated in most colon cancers, some cancers have increased ¦Â-catenin because of mutations in ¦Â-catenin (CTNNB1) that block its own breakdown, or have mutations in other genes with function similar to APC such as AXIN1, AXIN2, TCF7L2, or NKD1.
Beyond the defects in the Wnt signaling pathway, other mutations must occur for the cell to become cancerous. The p53 protein, produced by the TP53 gene, normally monitors cell division and killscells if they have Wnt pathway defects. Eventually, a cell line acquires a mutation in the TP53 gene and transforms the tissue from a benign epithelial tumor into an invasive epithelial cell cancer. Sometimes the gene encoding p53 is not mutated, but another protective protein named BAX is mutated instead.
Other proteins responsible for programmed cell death that are commonly deactivated in colorectal cancers are TGF-¦Â and DCC (Deleted in Colorectal Cancer). TGF-¦Â has a deactivating mutation in at least half of colorectal cancers. Sometimes TGF-¦Â is not deactivated, but a downstream protein named SMAD is deactivated. DCC commonly has a deleted segment of a chromosome in colorectal cancer.
Approximately 70% of all human genes are expressed in colorectal cancer, with just over 1% of having increased expression in colorectal cancer compared to other forms of cancer. Some genes areoncogenes: they are overexpressed in colorectal cancer. For example, genes encoding the proteins KRAS, BRAF, and PIK3CA, which normally stimulate the cell to divide in response to growth factors, can acquire mutations that result in over-activation of cell proliferation. The chronological order of mutations is sometimes important. If a previous APC mutation occurred, a primary KRAS mutation often progresses to cancer rather than a self-limiting hyperplastic or borderline lesion. PTEN, a tumor suppressor, normally inhibits PI3K, but can sometimes become mutated and deactivated.
Comprehensive, genome-scale analysis has revealed that colorectal carcinomas can be categorized into hypermutated and non-hypermutated tumor types. In addition to the oncogenic and inactivating mutations described for the genes above, non-hypermutated samples also contain mutated CTNNB1, FAM123B, SOX9, ATM, and ARID1A. Progressing through a distinct set of genetic events, hypermutated tumors display mutated forms of ACVR2A, EGFR, MSH3, MSH6, SLC9A9,TCF7L2, andBRAF. The common theme among these genes, across both tumor types, is their involvement in WNT and TGF-¦Â signaling pathways, which results in increased activity of MYC, a central player in colorectal cancer.
Risk factor of Colorectal cancer
Several lifestyle-related factors have been linked to colorectal cancer. In fact, the links between diet, weight, and exercise and colorectal cancer risk are some of the strongest for any type of cancer.
Being overweight or obese
If you are overweight or obese (very overweight), your risk of developing and dying from colorectal cancer is higher. Being overweight (especially having a larger waistline) raises the risk of colon cancer in both men and women, but the link seems to be stronger in men.
Physical inactivity
If you are not physically active, you have a greater chance of developing colorectal cancer. Being more active might help lower your risk.
Certain types of diets
A diet that is high in red meats (such as beef, pork, lamb, or liver) and processed meats (such as hot dogs and some luncheon meats) can raise your colorectal cancer risk.
Cooking meats at very high temperatures (frying, broiling, or grilling) creates chemicals that might raise your cancer risk, but it’s not clear how much this might increase your colorectal cancer risk.
Diets high in vegetables and fruits, and whole grain fibers have been linked with a lower risk of colorectal cancer, but fiber supplements have not been shown to help.
It’s not clear if other dietary components (for example, certain types of fats) affect colorectal cancer risk.
Smoking
People who have smoked for a long time are more likely than non-smokers to develop and die from colorectal cancer. Smoking is a well-known cause of lung cancer, but it is also linked to other cancers, like colorectal cancer. If you smoke and want to know more about quitting, see Guide to Quitting Smoking.
Heavy alcohol use
Colorectal cancer has been linked to heavy alcohol use. Limiting alcohol use to no more than 2 drinks a day for men and 1 drink a day for women could have many health benefits, including a lower risk of colorectal cancer.
Symptoms of Colorectal cancer
The signs and symptoms of colorectal cancer depend on the location of the tumor in the bowel, and whether it has spread elsewhere in the body (metastasis). The classic warning signs include: worsening constipation, blood in the stool, decrease in stool caliber (thickness), loss of appetite, loss of weight, and nausea orvomiting in someone over 50 years old. While rectal bleeding or anemia are high-risk features in those over the age of 50, other commonly described symptoms including weight loss and change in bowel habit are typically only concerning if associated with bleeding.
Diagnosis & Tests
The American Cancer Society believes that preventing colorectal cancer (and not just finding it early) should be a major reason for getting tested. Having polyps found and removed keeps some people from getting colorectal cancer. You are encouraged to have tests that have the best chance of finding both polyps and cancer if these tests are available to you and you are willing to have them. But the most important thing is to get tested, no matter which test you choose.
Starting at age 50, men and women at average risk for developing colorectal cancer should use one of the screening tests below:
Tests that find polyps and cancer
- item Colonoscopy every 10 years
- item CT colonography (virtual colonoscopy) every 5 years
- item Flexible sigmoidoscopy every 5 years
- item Double-contrast barium enema every 5 years
Tests that mainly find cancer
- item Fecal immunochemical test (FIT) every year
- item Guaiac-based fecal occult blood test (gFOBT) every year
- item Stool DNA test every 3 years*
If you are at an increased or high risk of colorectal cancer, you might need to start colorectal cancer screening before age 50 and/or be screened more often. The following conditions make your risk higher than average:
- item A personal history of colorectal cancer or adenomatous polyps
- item A strong family history of colorectal cancer or polyps
- item A known family history of a hereditary colorectal cancer syndrome such as familial adenomatous polyposis (FAP) or Lynch syndrome (hereditary non-polyposis colon cancer or HNPCC)
Stage of Colorectal cancer
After someone is diagnosed with colorectal cancer, doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it. Doctors also use a cancer's stage when talking about survival statistics.
The earliest stage colorectal cancers are called stage 0 (a very early cancer), and then range from stages I (1) through IV (4). As a rule, the lower the number, the less the cancer has spread. A higher number, such as stage IV, means cancer has spread more. And within a stage, an earlier letter means a lower stage. Although each person’s cancer experience is unique, cancers with similar stages tend to have a similar outlook and are often treated in much the same way.
Treatment
he treatment of colorectal cancer can be aimed at cure or palliation. The decision on which aim to adopt depends on various factors, including the person's health and preferences, as well as the stage of the tumor. When colorectal cancer is caught early, surgery can be curative. However, when it is detected at later stages (for which metastases are present), this is less likely and treatment is often directed at palliation, to relieve symptoms caused by the tumour and keep the person as comfortable as possible.
Surgery
If the cancer is found at a very early stage, it may be removed during a colonoscopy. For people with localized cancer, the preferred treatment is complete surgical removal with adequate margins, with the attempt of achieving a cure. This can either be done by an open laparotomy or sometimes laparoscopically. The colon may then be reconnected or a person may have a colostomy.
If there are only a few metastases in the liver or lungs they may also be removed. Sometimes chemotherapy is used before surgery to shrink the cancer before attempting to remove it. The two most common sites of recurrence of colorectal cancer are the liver and lungs.
Chemotherapy
In both cancer of the colon and rectum, chemotherapy may be used in addition to surgery in certain cases. The decision to add chemotherapy in management of colon and rectal cancer depends on the stage of the disease.
In Stage I colon cancer, no chemotherapy is offered, and surgery is the definitive treatment. The role of chemotherapy in Stage II colon cancer is debatable, and is usually not offered unless risk factors such as T4 tumor or inadequate lymph node sampling is identified. It is also known that the people who carry abnormalities of the mismatch repair genes do not benefit from chemotherapy. For stage III and Stage IV colon cancer, chemotherapy is an integral part of treatment.
If cancer has spread to the lymph nodes or distant organs, which is the case with stage III and stage IV colon cancer respectively, adding chemotherapy agentsfluorouracil, capecitabine or oxaliplatin increases life expectancy. If the lymph nodes do not contain cancer, the benefits of chemotherapy are controversial. If the cancer is widely metastatic or unresectable, treatment is then palliative. Typically in this setting, a number of different chemotherapy medications may be used. Chemotherapy drugs for this condition may include capecitabine, fluorouracil, irinotecan, oxaliplatin and UFT. The drugs capecitabine and fluorouracil are interchangeable, with capecitabine being an oral medication while fluorouracil being an intravenous medicine. Some specific regimens used for CRC are FOLFOX,FOLFOXIRI, and FOLFIRI. Antiangiogenic drugs such as bevacizumab are often added in first line therapy. Another class of drugs used in the second line setting are epidermal growth factor receptor inhibitors, of which the two FDA approved ones are cetuximab and panitumumab.
The primary difference in the approach to low stage rectal cancer is the incorporation of radiation therapy. Often, it is used in conjunction with chemotherapy in a neoadjuvant fashion to enable surgical resection, so that ultimately as colostomy is not required. However, it may not be possible in low lying tumors, in which case, a permanent colostomy may be required. Stage IV rectal cancer is treated similar to stage IV colon cancer.
Radiation therapy
While a combination of radiation and chemotherapy may be useful for rectal cancer, its use in colon cancer is not routine due to the sensitivity of the bowels to radiation. Just as forchemotherapy, radiotherapy can be used in the neoadjuvant and adjuvant setting for some stages of rectal cancer.
Immunotherapy
Immunotherapy with immune checkpoint inhibitors has been found to be useful for a type of colorectal cancer with mismatch repair deficiency and microsatellite instability. Most people who do improve, however, still worsen after months or years. Other types of colorectal cancer as of 2017 is still being studied.
Targeted therapy
Vascular endothelial growth factor (VEGF) is a protein that helps tumors form new blood vessels to get nutrients (a process known as angiogenesis). Drugs that stop VEGF from working can be used to treat some colon or rectal cancers. These include: Bevacizumab (Avastin) ,Ramucirumab (Cyramza),Ziv-aflibercept (Zaltrap)
Epidermal growth factor receptor (EGFR) is a protein that often appears in high amounts on the surface of cancer cells and helps them grow. Drugs that target EGFR can be used to treat some advanced colon or rectal cancers. These include: Cetuximab (Erbitux),Panitumumab (Vectibix)。
Some colorectal cancers have mutations (defects) in the KRAS, NRAS or BRAF gene, which make these drugs ineffective. Doctors now commonly test the tumor for these gene changes before treatment, and only use these drugs in people who do not have these mutations.
Regorafenib (Stivarga) is a type of targeted therapy known as a kinase inhibitor. Kinases are proteins on or near the surface of a cell that carry important signals to the cell’s control center. Regorafenib blocks several kinase proteins that either help tumor cells grow or help form new blood vessels to feed the tumor. Blocking these proteins can help stop the growth of cancer cells.
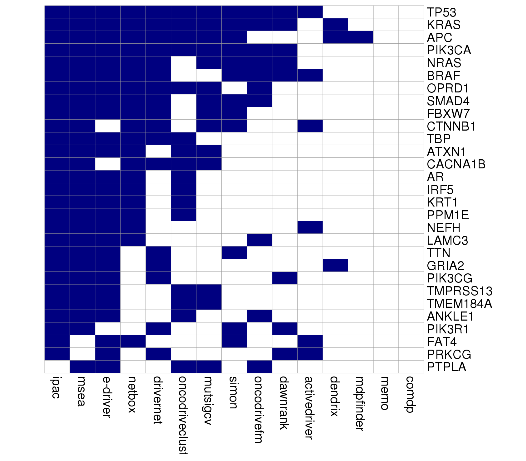
Colorectal cancer related genes
Colorectal cancer Drugs
Colorectal cancer Clinical Trials
You can ask your doctor to help you find a clinical trial, what’s involved, and what to consider -- for instance, if you’d need to travel to take part. You can also check these websites for information.
Eviti Clinical Trials
This website, developed by the nonprofit Coalition of Cancer Cooperative Groups, is the leading cancer clinical trial search engine. You can search for cancer trials based on disease and location.
National Cancer Institute
This website lists more than 6,000 cancer clinical trials and explains what to do when you find one that you think is right for you.
ClinicalTrials.gov
This website, a service of the National Institutes of Health, is a database of clinical studies worldwide.
CenterWatch
This web site lists industry-sponsored clinical trials that are recruiting patients.
Side Effects
Targeted therapy
Common side effects of these drugs include high blood pressure, tiredness, bleeding, low white blood cell counts (with increased risk of infections), headaches, mouth sores, loss of appetite, and diarrhea.
Surgery
Pain and weakness. Your doctor will prescribe medication to relieve your pain, but you’ll need to allow time to rest and heal. It’s a good idea to keep a journal so you can track and describe your symptoms. If it gets worse, work with your doctor to adjust medications and fine-tune the dosage.
Chemotherapy
Shortness of breath. You may feel this even though you’re getting enough oxygen and you can breathe normally. It’s how your brain processes chest pain. It should get better overthe next few weeks as you heal. If your lungs are in good shape (other than the cancer) you can usually return to normal life after a while -- even if an entire lung was removed. If you also have a non-cancerous lung disease like emphysema or chronic bronchitis, you may always feel short of breath with some types of activity.
Nausea and vomiting. Feeling like you're going to throw up or actually doing it can be a problem on treatment days. Your doctor will give you medicine to keep these symptoms at bay.
Hair loss. Follicles, the tiny structures that hair grows out of, contain some of the fastest-growing cells in your body. So chemo attacks them, too. Within a few weeks of starting treatment, you may lose some or all of your hair. The good news is that it's almost always temporary. It can make you feel better to cut or shave before it starts to fall out. If you opt to go bald, use an electric shaver so you don't cut your scalp. If you get a wig, shop for it while you still have hair so you can match it to your current hair color.
Bleeding or clotting problems. Platelets are blood cells that help stop bleeding. They plug damaged blood vessels and help your blood clot. If you don't have enough of them, you may bleed or bruise more easily than usual, even from a minor injury. Your doctor will check your platelet count often during your treatment. If it falls too low, you may need a transfusion.
Loss of appetite. Instead of three large meals per day, have five or six small ones. Avoid greasy, salty, sweet, or spicy food that might make you feel queasy. If even the smell of food is a turnoff, eat cold meals instead.
Diarrhea. Frequent bowel movements that are loose or watery can get in the way of your daily life. They can also drain too much liquid from your body. Skip dairy and high-fiber, greasy, or spicy foods. Drink water or suck on ice chips, and call you doctor if your symptoms last more than a day.
Radiation Therapy
- item Shortness of breath
- item Fatigue
- item Nausea and vomiting
- item Diarrhea
- item Hair loss
- item Loss of appetite
- item Skin changes in the area being treated.
- item Sore throat.
Nutrition of the patients
Eating well is important before, during, and after cancer treatment. You need the right amount of calories to maintain a good weight. You also need enough protein to keep up your strength. Eating well may help you feel better and have more energy.
Sometimes, especially during or soon after treatment, you may not feel like eating. You may be uncomfortable or tired. You may find that foods don’t taste as good as they used to. In addition, poor appetite, nausea, vomiting, mouth blisters, and other side effects of treatment can make it hard for you to eat.
Follow-up Care
You’ll need regular checkups (such as every 6 months) after treatment for lung cancer. Checkups help ensure that any changes in your health are noted and treated if needed. If you have any health problems between checkups, contact your doctor.
Lung cancer may come back after treatment. Your doctor will check for the return of cancer. It may return in the chest or it may return in another part of the body, such as the bones.
Checkups also help detect health problems that can result from cancer treatment.
Checkups may include a physical exam, blood tests, or CT scans.