Breast cancer
Breast cancer
What is Breast Cancer
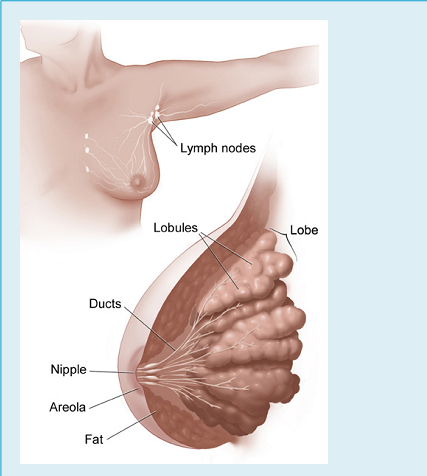
Inside a woman's breast are 15 to 20 sections (lobes). Each lobe is made of many smaller sections (lobules). Lobules have groups of tiny glands that can make milk.
After a baby is born, breast milk flows from the lobules through thin tubes (ducts) to the nipple. Fibrous tissue and fat fill the spaces between the lobules and ducts.
Cancer begins in cells, the building blocks that make up all tissues and organs of the body, including the breast.
Normal cells in the breast and other parts of the body grow and divide to form new cells as they are needed. When normal cells grow old or get damaged, they die, and new cells take their place.
Sometimes, this process goes wrong. New cells form when the body doesn't need them, and old or damaged cells don't die as they should. The buildup of extra cells often forms a mass of tissue called a lump, growth, or tumor.
Tumors in the breast can be # benign (not cancer) or malignant (cancer):
Benign tumors
- item Are rarely a threat to life
- item Don't invade the tissues around them
- item Don't spread to other parts of the body
- item Usually don't need to be removed
Malignant tumors (breast cancer)
- item May be a threat to life
- item Can invade nearby organs and tissues
- item Can spread to other parts of the body
- item Often can be removed but may grow back
Breast cancer cells can spread by breaking away from a breast tumor. They can travel through blood vessels or lymph vessels to reach other parts of the body. After to form new tumors that may damage those tissues.
For example, breast cancer cells may spread first to nearby lymph nodes. Groups of lymph nodes are near the breast under the arm (axilla), above the collarbone, and in the chest behind the breastbone.
When breast cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the primary (original) tumor. For example, if breast cancer spreads to a lung, the cancer cells in the lung are actually breast cancer cells. The disease is metastatic breast cancer, not lung cancer. For that reason, it's treated as breast cancer, not lung cancer.
Types of Breast Cancer
The most common type of breast cancer is ductal carcinoma. This cancer begins in cells that line a breast duct. See page 1 for a picture of breast ducts. About 7 of every 10 women with breast cancer have ductal carcinoma.
The second most common type of breast cancer is lobular carcinoma. This cancer begins in a lobule of the breast. See page 1 for a picture of lobules. About 1 of every 10 women with breast cancer has lobular carcinoma.
Other women have a mixture of ductal and lobular type or they have a less common type of breast cancer.
Molecular classification
There are five main intrinsic or molecular subtypes of breast cancer that are based on the genes a cancer expresses:
Luminal A
Breast cancer is hormone-receptor positive (estrogen-receptor and/or progesterone-receptor positive), HER2 negative, and has low levels of the protein Ki-67, which helps control how fast cancer cells grow. Luminal A cancers are low-grade, tend to grow slowly and have the best prognosis.
Luminal B
Breast cancer is hormone-receptor positive (estrogen-receptor and/or progesterone-receptor positive), and either HER2 positive or HER2 negative with high levels of Ki-67. Luminal B cancers generally grow slightly faster than luminal A cancers and their prognosis is slightly worse.
Triple-negative/basal-like
Breast cancer is hormone-receptor negative (estrogen-receptor and progesterone-receptor negative) and HER2 negative. This type of cancer is more common in women with BRCA1 gene mutations. Researchers aren't sure why, but this type of cancer also is more common among younger and African-American women.
HER2-enriched
Breast cancer is hormone-receptor negative (estrogen-receptor and progesterone-receptor negative) and HER2 positive. HER2-enriched cancers tend to grow faster than luminal cancers and can have a worse prognosis, but they are often successfully treated with targeted therapies aimed at the HER2 protein, such as Herceptin (chemical name: trastuzumab), Perjeta (chemical name: pertuzumab), Tykerb (chemical name: lapatinib), and Kadcyla (chemical name: T-DM1 or ado-trastuzumab emtansine).
Normal-like
Breast cancer is similar to luminal A disease: hormone-receptor positive (estrogen-receptor and/or progesterone-receptor positive), HER2 negative, and has low levels of the protein Ki-67, which helps control how fast cancer cells grow. Still, while normal-like breast cancer has a good prognosis, its prognosis is slightly worse than luminal A cancer's prognosis.
Risk factor of Breast Cancer
Risk factors can be divided into two categories:
- item modifiable risk factors (things that people can change themselves, such as consumption of alcoholic beverages), and
- item fixed risk factors (things that cannot be changed, such as age and biological sex).
The primary risk factors for breast cancer are being female and older age. Other potential risk factors include genetics, lack of childbearing or lack of breastfeeding, higher levels of certain hormones, certain dietary patterns, and obesity. Recent studies have indicated that exposure to light pollution is a risk factor for the development of breast cancer.
Lifestyle
Smoking tobacco appears to increase the risk of breast cancer, with the greater the amount smoked and the earlier in life that smoking began, the higher the risk. In those who are long-term smokers, the risk is increased 35% to 50%.
The association between breast feeding and breast cancer has not been clearly determined; some studies have found support for an association while others have not. In the 1980s, the abortion–breast cancer hypothesis posited that induced abortion increased the risk of developing breast cancer. This hypothesis was the subject of extensive scientific inquiry, which concluded that neither miscarriages nor abortions are associated with a heightened risk for breast cancer.
A number of dietary factors have been linked to the risk for breast cancer. Dietary factors which may increase risk include a high fat diet, high alcohol intake, and obesity-related high cholesterol levels. Dietary iodine deficiency may also play a role. Evidence for fiber is unclear. A 2015 review found that studies trying to link fiber intake with breast cancer produced 3mixed results. In 2016 a tentative association between low fiber intake during adolescence and breast cancer was observed.
Other risk factors include radiation and shift-work. A number of chemicals have also been linked, including polychlorinated biphenyls, polycyclic aromatic hydrocarbons, and organic solvents. Although the radiation from mammography is a low dose, it is estimated that yearly screening from 40 to 80 years of age will cause approximately 225 cases of fatal breast cancer per million women screened.
Genetics
Some genetic susceptibility may play a minor role in most cases. Overall, however, genetics is believed to be the primary cause of 5–10% of all cases. Women whose mother was diagnosed before 50 have an increased risk of 1.7 and those whose mother was diagnosed at age 50 or after has an increased risk of 1.4. In those with zero, one or two affected relatives, the risk of breast cancer before the age of 80 is 7.8%, 13.3%, and 21.1% with a subsequent mortality from the disease of 2.3%, 4.2%, and 7.6% respectively. In those with a first degree relative with the disease the risk of breast cancer between the age of 40 and 50 is double that of the general population.
Medical conditions
Breast changes like atypical ductal hyperplasia and lobular carcinoma in situ, found in benign breast conditions such as fibrocystic breast changes, are correlated with an increased breast cancer risk. Diabetes mellitus might also increase the risk of breast cancer. Autoimmune diseases such aslupus erythematosus seem also to increase the risk for the acquisition of breast cancer.
Symptoms of Breast Cancer
The most common symptom of breast cancer is a new lump or mass. A painless, hard mass that has irregular edges is more likely to be cancer, but breast cancers can be tender, soft, or rounded. They can even be painful. For this reason, it is important to have any new breast mass, lump, or breast change checked by a health care professional experienced in diagnosing breast diseases.
Other possible symptoms of breast cancer include:
- item Swelling of all or part of a breast (even if no distinct lump is felt)
- item Skin irritation or dimpling (sometimes looking like an orange peel)
- item Breast or nipple pain
- item Nipple retraction (turning inward)
- item Redness, scaliness, or thickening of the nipple or breast skin
- item Nipple discharge (other than breast milk)
Sometimes a breast cancer can spread to lymph nodes under the arm or around the collar bone and cause a lump or swelling there, even before the original tumor in the breast is large enough to be felt. Swollen lymph nodes should also be checked by a health care provider.
Although any of these symptoms can be caused by things other than breast cancer, if you have them, they should be reported to a health care professional so that the cause can be found.
Because mammograms do not find every breast cancer, it is important for you to be aware of changes in your breasts and to know the signs and symptoms of breast cancer.
Diagnosis & Tests
The breast tissue that was removed during your biopsy can be used in special lab tests:
Hormone receptor tests: Some breast cancers need hormones to grow. These cancers have hormone receptors for the hormones estrogen, progesterone, or both. If the hormone receptor tests show that the breast cancer has these receptors, then hormone therapy is often recommended as part of the treatment plan.
HER2 test: Some breast cancers have large amounts of a protein called HER2, which helps them to grow. The HER2 test shows whether a woman's breast cancer has a large amount of HER2. If so, then targeted therapy against HER2 may be a treatment option.
It may take several weeks to get the results of these tests. The test results help your doctor decide which cancer treatments may be options for you.
Stage of Breast Cancer
The stage of breast cancer depends on the size of the breast tumor and whether it has spread to lymph nodes or other parts of the body.
Doctors describe the stages of breast cancer using the Roman numerals 0, I, II, III, and IV and the letters A, B, and C.
A cancer that is Stage I is early-stage breast cancer, and a cancer that is Stage IV is advanced cancer that has spread to other parts of the body, such as the liver.
The stage often is not known until after surgery to remove the tumor in the breast and one or more underarm lymph nodes.
Stage 0
Stage 0 is carcinoma in situ. In ductal carcinoma in situ (DCIS), abnormal cells are in the lining of a breast duct, but the abnormal cells have not invaded nearby breast tissue or spread outside the duct.
Stage IA
The breast tumor is no more than 2 centimeters (no more than 3/4 of an inch) across. Cancer has not spread to the lymph nodes.
Stage IB
The tumor is no more than 2 centimeters across. Cancer cells are found in lymph nodes.
Stage IIA
The tumor is no more than 2 centimeters across, and the cancer has spread to underarm lymph nodes.
Or, the tumor is between 2 and 5 centimeters (between 3/4 of an inch and 2 inches) across, but the cancer hasn't spread to underarm lymph nodes.
Stage IIB
The tumor is between 2 and 5 centimeters across, and the cancer has spread to underarm lymph nodes.
Or, the tumor is larger than 5 centimeters across, but the cancer hasn't spread to underarm lymph nodes.
Stage IIIA
The breast tumor is no more than 5 centimeters across, and the cancer has spread to underarm lymph nodes that are attached to each other or nearby tissue. Or, the cancer may have spread to lymph nodes behind the breastbone.
Or, the tumor is more than 5 centimeters across. The cancer has spread to underarm lymph nodes that may be attached to each other or nearby tissue. Or, the cancer may have spread to lymph nodes behind the breastbone but not spread to underarm lymph nodes.
Stage IIIB
The breast tumor can be any size, and it has grown into the chest wall or the skin of the breast. The breast may be swollen or the breast skin may have lumps.
The cancer may have spread to underarm lymph nodes, and these lymph nodes may be attached to each other or nearby tissue. Or, the cancer may have spread to lymph nodes behind the breastbone.
Stage IIIC
The breast cancer can be any size, and it has spread to lymph nodes behind the breastbone and under the arm. Or, the cancer has spread to lymph nodes above or below the collarbone.
Stage IV
The tumor can be any size, and cancer cells have spread to other parts of the body, such as the lungs, liver, bones, or brain.
Treatment
Women with breast cancer have many treatment options. Treatment options include:
Surgery
Surgery is the most common treatment for breast cancer. There are several kinds of surgery.
Your surgeon can describe each kind of surgery, compare the benefits and risks, and help you decide which kind might be best for you:
Removing part of the breast: Breast-sparing surgery is an operation to remove the cancer and a small amount of the normal tissue that surrounds it. This is also called breast-conserving surgery. It can be a lumpectomy or a segmental mastectomy (also called a partial mastectomy). A woman usually has radiation therapy after breast-sparing surgery to kill cancer cells that may remain in the breast area.
Some women will have more tissue removed but not the whole breast. For these women, the surgeon will remove lymph nodes under the arm and some of the lining over the chest muscles below the tumor.
Removing the whole breast: Surgery to remove the whole breast (or as much of the breast tissue as possible) is a mastectomy. In some cases, a skin-sparing mastectomy may be an option. For this approach, the surgeon removes as little skin as possible.
Radiation therapy
Radiation therapy uses high-energy rays to kill cancer cells. It affects cells only in the part of the body that is treated.
Radiation therapy may be used after surgery to destroy breast cancer cells that remain in the chest area. Women usually have radiation therapy after breast-sparing surgery, but it's sometimes used after mastectomy too.
You can get radiation therapy to treat breast cancer in two ways:
Machine outside the body (external radiation therapy): The radiation comes from a large machine outside the body. You'll go to a hospital or clinic for treatment. Usually, women get treatment once a day, 5 days a week for 3 to 6 weeks. Each treatment session lasts only a few minutes. External radiation is the most common type used for breast cancer.
Material inside the body (brachytherapy): The doctor will place one or more thin tubes inside the breast through a tiny incision. A radioactive substance is loaded into the tube. The treatment session may last for a few minutes, and the substance is removed. When it's removed, no radioactivity remains in your body. This method of radiation therapy may be repeated every day for a week.
Side effects depend mainly on the type of radiation and how much is given. Ask your health care team to describe what you can expect.
Hormone therapy
Hormone therapy can also be called anti-hormone treatment. If lab tests show that your breast cancer cells have hormone receptors, then hormone therapy may be an option. (See the part about Lab Tests with Breast Tissue on page 4.) Hormone therapy keeps the cancer cells from getting or using the natural hormones (estrogen and progesterone) they need to grow.
If you have not gone through menopause, the options for hormone therapy include:
A drug that blocks estrogen's activity in the body (tamoxifen)
Surgery to remove your ovaries (which make estrogen)
A drug that reduces the amount of estrogen made by the ovaries (LH-RH agonist)
If you have gone through menopause, the options include:
A drug that prevents the body from making estrogen (aromatase inhibitor)
Tamoxifen
The side effects of hormone therapy depend on the type used. The most common side effects are hot flashes, vaginal discharge, and nausea.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. It may be given to women with Stage I, II, III, or IV breast cancer. Chemotherapy may be given before or after surgery.
The drugs for breast cancer are usually given directly into a vein (intravenously) through a thin needle or as a pill. You may receive a combination of drugs.
You may receive chemotherapy in a clinic, at the doctor's office, or at home. It's unusual for a woman to need to stay in the hospital during treatment.
The side effects depend mainly on which drugs are given and how much. Chemotherapy kills fast-growing cancer cells, but the drugs can also harm normal cells that divide rapidly:
Blood cells: When drugs lower the levels of healthy blood cells, you're more likely to get infections, bruise or bleed easily, and feel very weak and tired. Your health care team will check for low levels of blood cells. If your levels are low, your health care team may stop the chemotherapy for a while or reduce the dose of the drug. There are also medicines that can help your body make new blood cells.
Cells in hair roots: Chemotherapy may cause hair loss. If you lose your hair, it will grow back after treatment, but the color and texture may be changed.
Cells that line the digestive tract: Chemotherapy can cause a poor appetite, nausea and vomiting, diarrhea, or mouth and lip sores. Your health care team can give you medicines and suggest other ways to help with these problems.
Targeted therapy
Women whose lab tests show that their breast cancer cells have too much HER2 protein may receive targeted therapy. The targeted therapies used to treat breast cancer block cancer cell growth by blocking the action of the extra HER2 protein.
These drugs may be given intravenously or as a pill. The side effects depend mainly on which drug is given. Possible side effects include nausea, vomiting, and diarrhea. The drugs may also cause heart damage, heart failure, and serious breathing problems. During treatment, your doctor will watch for signs of heart and lung problems.
The treatment that's best for one woman may not be best for another. The treatment that's right for you depends mainly on:
- item The stage of breast cancer
- item Whether the tumor has hormone receptors
- item Whether the tumor has too much HER2
- item Your general health
In addition, your treatment plan depends on:
- item The size of the tumor in relation to the size of your breast
- item Whether you have gone through menopause
Breast Cancer related genes
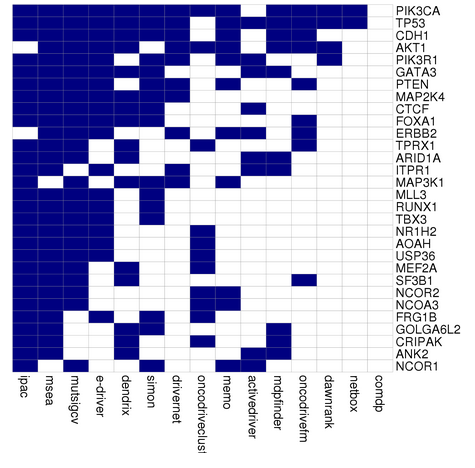
In less than 5% of cases, genetics plays a more significant role by causing a hereditary breast–ovarian cancer syndrome. This includes those who carry the BRCA1 and BRCA2 gene mutation. These mutations account for up to 90% of the total genetic influence with a risk of breast cancer of 60–80% in those affected. Other significant mutations include p53 (Li–Fraumeni syndrome), PTEN PTEN (Cowden syndrome), and STK11(Peutz–Jeghers syndrome), CHEK2, ATM, BRIP1, and PALB2. In 2012, researchers said that there are four genetically distinct types of the breast cancer and that in each type, hallmark genetic changes lead to many cancers.
Breast Cancer Drugs
Breast Cancer Clinical Trials
Clinical trials are a way to try new medications and treatments that researchers are testing. The goal is to find out how well these treatments work and what side effects they could have.
People with breast cancer who participate in breast cancer clinical trials get the most effective therapy that's already available, or they may receive new breast cancer treatments that are being tested for future use.
You can ask your doctor to help you find a clinical trial, what's involved, and what to consider -- for instance, if you'd need to travel to take part. You can also check these websites for information.
Eviti Clinical Trials
This website, developed by the nonprofit Coalition of Cancer Cooperative Groups, is the leading cancer clinical trial search engine. You can search for cancer trials based on disease and location.
National Cancer Institute
This website lists more than 6,000 cancer clinical trials and explains what to do when you find one that you think is right for you.
ClinicalTrials.gov
This website, a service of the National Institutes of Health, is a database of clinical studies worldwide.
CenterWatch
This web site lists industry-sponsored clinical trials that are recruiting patients.
Side Effects
Your health care team can describe your treatment options, the expected results of each option, and the possible side effects. Because cancer treatments often damage healthy cells and tissues, side effects are common. These side effects depend on many factors, including the type of treatment.
As you get ready to start treatment, it's normal to feel nervous about side effects you might face. To help you prepare, here's a treatment-by-treatment guide to the most common ones.
Keep in mind that side effects vary even between two people on the same treatment. That's because every person -- and every cancer case -- is unique. The good news is most side effects are temporary and there are ways you can manage them.
Surgery
Pain and weakness. Your doctor will prescribe medication to relieve your pain, but you'll need to allow time to rest and heal. It's a good idea to keep a journal so you can track and describe your symptoms. If it gets worse, work with your doctor to adjust medications and fine-tune the dosage.
Chemotherapy
Shortness of breath. You may feel this even though you're getting enough oxygen and you can breathe normally. It's how your brain processes chest pain. It should get better over the next few weeks as you heal. If your breast are in good shape (other than the cancer) you can usually return to normal life after a while -- even if an entire breast was removed. If you also have a non-cancerous disease like emphysema or chronic bronchitis, you may always feel short of breath with some types of activity.
Nausea and vomiting. Feeling like you're going to throw up or actually doing it can be a problem on treatment days. Your doctor will give you medicine to keep these symptoms at bay.
Hair loss. Follicles, the tiny structures that hair grows out of, contain some of the fastest-growing cells in your body. So chemo attacks them, too. Within a few weeks of starting treatment, you may lose some or all of your hair. The good news is that it's almost always temporary. It can make you feel better to cut or shave before it starts to fall out. If you opt to go bald, use an electric shaver so you don't cut your scalp. If you get a wig, shop for it while you still have hair so you can match it to your current hair color.
Bleeding or clotting problems. Platelets are blood cells that help stop bleeding. They plug damaged blood vessels and help your blood clot. If you don't have enough of them, you may bleed or bruise more easily than usual, even from a minor injury. Your doctor will check your platelet count often during your treatment. If it falls too low, you may need a transfusion.
Loss of appetite. Instead of three large meals per day, have five or six small ones. Avoid greasy, salty, sweet, or spicy food that might make you feel queasy. If even the smell of food is a turnoff, eat cold meals instead.
Diarrhea. Frequent bowel movements that are loose or watery can get in the way of your daily life. They can also drain too much liquid from your body. Skip dairy and high-fiber, greasy, or spicy foods. Drink water or suck on ice chips, and call you doctor if your symptoms last more than a day.
Nutrition of the patients
Eating well is important before, during, and after cancer treatment. You need the right amount of calories to maintain a good weight. You also need enough protein to keep up your strength. Eating well may help you feel better and have more energy.
Sometimes, especially during or soon after treatment, you may not feel like eating. You may be uncomfortable or tired. You may find that foods don't taste as good as they used to. In addition, poor appetite, nausea, vomiting, mouth blisters, and other side effects of treatment can make it hard for you to eat. On the other hand, some women treated for breast cancer may have a problem with weight gain.
Follow-up Care
You'll need regular checkups (such as every 3 to 6 months) after treatment for breast cancer. Checkups help ensure that any changes in your health are noted and treated if needed. If you have any health problems between checkups, contact your doctor.
Breast cancer that comes back after treatment: Breast cancer may return in the breast or chest wall. Or, it may return in any other part of the body, such as the bones, liver, lungs, or brain.
Health problems that can result from cancer treatment
A new breast cancer
Checkups usually include an exam of the neck, underarm, chest, and breast areas. Since a new breast cancer may develop, you should have regular mammograms. You probably won't need a mammogram of a reconstructed breast or if you had a mastectomy without reconstruction. Your doctor may order other imaging procedures or lab tests.
Breast Reconstruction
A woman who plans to have a mastectomy has a choice about whether or not to have surgery to rebuild the shape of the breast (breast reconstruction). Instead of breast reconstruction, a woman could choose to wear a breast form (a device that replaces the breast), wear padding inside her bra, or do nothing. All of these options have pros and cons. What is right for one woman may not be right for another.
Breast reconstruction may be done at the same time as the mastectomy, or it may be done later on. If radiation therapy is part of the treatment plan, some doctors suggest waiting until after radiation therapy is complete.
If you're thinking about breast reconstruction, talk to a plastic surgeon before the mastectomy, even if you plan to have your reconstruction later on.
A surgeon can reconstruct the breast in many ways. Some women choose to have breast implants, which are filled with saline or silicone gel.
Another method of breast reconstruction is to create a breast shape using tissue taken from another part of your body. The plastic surgeon can take skin, muscle, and fat from your lower abdomen, back, or buttocks.
The type of reconstruction that is best for you depends on your age, body type, and the type of cancer surgery that you had. A plastic surgeon can help you decide.